
The defibrillator, bellows and Bag Valve Mask on display at Crawley Museum to celebrate 75 years of the NHS.
As part of the celebrations of 75 years since the inception of the NHS I was asked to write a piece about the part of the NHS that I know most about. Being an “almost retired” Paramedic with 39 years’ experience, naturally my chosen subject was a small part of the development of the Ambulance Service since 1948. I have borrowed two historic Items from the collection of Surrey Ambulance Retirement Association (SARA) which tell the story of how prehospital resuscitation has developed as a key skill of the Ambulance Service. A snapshot of a critically important skill that can be the difference between life and death.
The NHS Ambulance Service since 1948

Line drawing of Ambulance Volantes or Flying Ambulances.
The modern concept of the ambulance as rapid transport to professional medical aid was established during the Napoleonic wars by Dominique Jean Larrey (1766 – 1842) Napoleon’s chief surgeon. Larrey recognised the need to treat casualties rapidly – particularly those who required amputation (to prevent sepsis) and the need to stem bleeding. He created a corps of “Ambulance Volantes” (Flying Ambulances) adapted from artillery gun carriages – replacing the guns with casualties.
In 1948 as part of the NHS act 1946 (Part 3 Section 27 parts 1&2) the ambulance service as we know it today was born. Prior to 1948 Ambulances were provided on a local, somewhat Ad Hoc basis by a combination of Volunteers such as the SJAB / Red Cross and Police and Fire Services and County Councils, where the Ambulance fleet was often managed by the same department as refuse collections. There was no regulation in relation to ambulance types, equipment, crew training or response times.
Effectively “on the ground” after the Act there was initially no change other than local Health Authorities were created to take responsibility for medical services including Ambulance provision. Ambulances could now be run directly by the Health Authorities themselves or continue to be “contracted” out to voluntary agencies and councils. The Role was, in the language of the day “the conveyance of persons suffering from illness or mental defectiveness or expectant or nursing mothers”.
As mentioned, there was no reference to what was expected to happen during that conveyance of patients/casualties. My late Mother (Rose) described her experience of being in a serious traffic collision in the 1950’s when she sustained head, chest, and maxillo-facial injuries (no seat belt or helmet laws in those days) and the ambulance crew that arrived comprised of a male driver and a young female Nurse. My mother was simply put on a stretcher, and the nurse remained in the back with her, in my mother’s words “looking terrified” and not doing anything. A national training syllabus was eventually to arrive with the Millar Report in 1966 which outlined the treatment that ambulance staff were expected to provide and marked a significant step in the provision of prehospital care. A local Crawley “ambulance man” (and much admired colleague) who joined prior to 1966 told me that he did a 2 week first aid course and reported to Crawley Ambulance station at 09.00hrs on the following Monday. At 09.10 he was on his way to his first emergency.
Prehospital Resuscitation

Image of a Tobacco Smoke Enema taking place.
Resuscitation is defined in the Oxford Dictionary as “the action or process of reviving someone from unconsciousness or apparent death” and there have been records of attempted resuscitation throughout history. Possibly one of the strangest forms of resuscitation (aimed at drowned casualties) was the infusion of tobacco smoke into rectum via the anus (Tobacco Smoke Enema) that was believed to stimulate breathing and warm the patient. There is very little evidence that it worked but it would have been interesting to see the look on the casualty’s face if they did recover. Pre Rectum (PR) is a route that is occasionally used in pre hospital emergency care to give sedatives to a fitting patient.
Most early resuscitative efforts centred around stimulating breathing, which is an observable and reassuring sign of life and paid little attention to what the heart was doing i.e., was it beating or not? Mouth to mouth ventilation had been performed in France in 1740 and cardiac compression first tried in 1891. Neither caught on at the time. In the 1950’s American doctors Elms and Safar combined mouth to mouth and chest compressions and created the now well-known ABC of resuscitation. A for airway, B for breathing and C for circulation which is still the basis of resuscitation to this day.
Breathing – The Porton Bellows 1950’s

Porton Bellows on display at Crawley Museum.

This is the military version with a filter between the bellows and the facemask to prevent chemical agents from contaminating the air delivered to the casualty.
The Porton Bellows was a respiratory device created at the Chemical Defence Experimental Establishment at Porton is Wiltshire. It was developed with the Cold War in mind and the possibility of chemical attack by Soviet Russia. Chemical (nerve) agents would paralyse the casualty, stop them breathing and they would die from asphyxiation, so the bellows were designed for rescuers to maintain breathing artificially while an antidote (Atropine) was administered.
Like many military medical devices, it clearly had civilian application and the example that was on display at the Museum was issued to Surrey Ambulance Service. From records it appears that one set of Porton Bellows was kept on each main station and would be requested when needed. Main Stations served 4 sub stations. In a pre-hospital resuscitation, the crew would have been expected to carry out mouth to mouth or one of the other ventilation techniques until the bellows arrived.
Apparently 8 years research went into the development of the bellows but on handling them they feel quite clumsy and the potential to over ventilate the casualty or ventilate with excessive pressure, which may cause other issues, seems high. This is the civilian version.

Instructions on how to use the bellows.
Breathing – Bag Valve Mask (BVM)

The BVM is the modern equivalent of the Porton Bellows and has significant advantages. As the name suggests it has a plastic bag that contains air which the operator squeezes to ventilate the patient, and which naturally returns to its open bag shape after each ventilation. A one-way valve allows air to pass through to a face mask – exhaled air is expelled by the valve. The kit comes with small medium and large face masks to allow for different facial anatomy. One size does not fit all which would have been a disadvantage of the Porton Bellows. And oxygen can be “entrained” through the system to increase oxygen delivery to the patient if required (vital in prolonged resuscitation). The kit also comes in child and infant sizes and is single use only to prevent cross infection.
Defibrillation

Defibrillation unit.
The other Item that I chose from the SARA collection is a Cardiac Monitor / Defibrillator probably one of the earliest ones designed for prehospital use in the 1970’s made by Cardiac Recorders (CR26) and for a portable device weighs 9Kg or 21 Lbs.
What is Defibrillation.
The Lungs allow blood to take oxygen from the air and the heart is a pump formed of cardiac muscle that pumps the oxygenated blood through the body and returns it to the lungs to expel Carbon Dioxide (CO2) a waste product of cell metabolism. The regular heartbeat is controlled by the electrical conduction system – specialised tissue within the heart muscle that generates an electrical impulse to coordinate the heartbeat. When a heart malfunctions the electrical conduction system loses control, and each individual muscle fibre starts to contract and relax independently of the ones around it – effectively it is in chaos and the heart can no longer co-ordinate to pump blood around the body. This is known as fibrillation and often referred to as “Cardiac Arrest” as the heart stops pumping effectively. If this is not corrected rapidly the brain loses its oxygenated blood supply and irreversible brain damage can occur within 4 – 5 minutes depending on how much oxygen is in the blood at the time of the cardiac arrest. Without chest compressions the fibrillation will diminish and stop completely.
Chest compressions can artificially move blood through the system (to the brain and the heart muscle itself) and artificial ventilation (BVM/Mouth to Mouth) can oxygenate the blood and ensure that the heart at least keeps fibrillating for a lot longer. A fibrillating heart has a better chance of survival – if it can be defibrillated.

In this image the “electrodes” used are buckets of salt solution – in the modern age they are small discs with gel to help conductivity. It is believed to be Dr Einthoven in the picture.
How do we know this? In 1890’s Willem Einthoven a Dutch doctor and physiologist discovered that the electrical impulse of the heart was powerful enough to be recorded at skin level and the Electrocardiogram (ECG) was born. This allows medics to interpret the electrical activity of the heart through electrodes placed on specific areas of the skin.

Comparison of the electrical activity in a normal heart, Normal Sinus Rhythm (NSR) which is regular and organised and has a wave formation that medics would recognise in relation to healthy heart activity and Fibrillation – more accurately called Ventricular Fibrillation (VF). The lack of coordination and inability to pump regularly in VF is plain to see.
The act of defibrillating is essentially passing a controlled electric impulse (shock) across the heart which causes one massive contraction of the heart and a short period of stillness (cardiac stunning) allowing the normal conduction system to cut back in and regain control.
In the mid-1960s Dr Frank Pantridge (during my research I discovered we went to the same school – I was a little after Frank) established a cardiac ambulance in Belfast. This was driven by the Ambulance Service but carried Dr Pantridge or one of his Registrar’s and a Coronary Care Nurse. He established that VF was more prevalent in the community than realised and that rapid defibrillation was the answer. The first “portable” defibrillator Dr Pantridge used weighed 70 Kg and ran off two car batteries. This experience led him to carry out a lot of research and eventually he created a portable defibrillator that weighed only 3Kg. Unfortunately, Dr Pantridges ideal of having a defibrillator on every ambulance (The Pantridge Plan) was still some time away.
Watch BBC 1969 report on Man Alive Cardiac ambulance here
Defibrillation in Sussex

Professor Douglas Chamberlain outside the old ambulance station next to Brighton General Hospital.
Meanwhile in Brighton (1970) a young cardiologist (from Cardiff) Dr Douglas Chamberlain (Now the highly respected Professor Chamberlain) was undoubtedly watching events in Belfast. After attending a Cardiac Arrest in the community (where the crude defibrillator exploded due to poor maintenance) he decided that he would train ambulance crews to defibrillate and to read ECG’s so that they could identify patients who were at increased risk of Ventricular Fibrillation. This certainly went against medical opinion of the time that Ambulance Crews would not have the ability to take on this type of training or deliver this level of emergency care.
Dr Chamberlain was a hard task master and developed a local course that was effectively the basis for a syllabus that was eventually taught nationally. Ambulance staff who had passed the course were often referred to colloquially as “Chamberlain men” (there were not many females in the service at that time) they were admired as they had to work hard to impress Dr Chamberlain. When Paramedics of today use the “10 rules of reading an ECG” they are in fact Dr Chamberlains 10 rules that their predecessors had to know by heart from 1971 onwards.
So, it is true to say that Sussex, was and has continued to be, at the forefront of pre hospital cardiac care thanks to this ”Welsh Son of Sussex”. I would also like to say that this description of Professor Chamberlains contribution merely skims the surface of an outstanding career and his massive influence on saving lives in the community and mention that Brighton’s new Ambulance Make Ready Centre (Station) is called Chamberlain House in his honour.
Defibrillation in Sussex Today
We have come a long way since the exploding defibrillator. Professional cardiac monitor defibrillators used by Paramedics can “read” ECG’s, use telemetry to send them to A&E, take blood pressure, establish the level of oxygen in the blood and analyse the level of CO2 in exhaled air in addition to providing a defibrillatory shock. Much more importantly, due to technological advances, Defibrillation is a now a lifesaving procedure that any member of the public can administer providing they have access to an Automated External Defibrillator or AED.
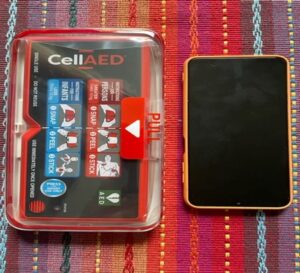
My own portable AED next to a standard mobile phone.
AEDs are lightweight defibrillators that anyone can use, you simply switch them on and follow the voice prompts. The AED simply needs a human to apply it and it then is able to analyse the heart rhythm and if required (i.e. the rhythm is VF) deliver a lifesaving defibrillatory shock. Defibrillation is more successful the sooner it is carried out hence the vital importance of having AEDs in our community that are accessible to the public. While training always helps give confidence it is not entirely necessary as the AED directs the user. Anyone can use an AED on someone in cardiac arrest as the device will only tell the user to deliver the shock (press a button) if that shock is needed. You cannot harm the patient. At the time of writing the Department of Health and Social Care is inviting organisations and community groups to bid for funds to purchase AED’s
I am willing to pass on my experience and train community groups to carry out basic resuscitation (CPR – Cardio Pulmonary Resuscitation) and use of AED’s free providing they have a venue.
John Battersby McPara, PgCert (Critical Care), CertEd.
Interesting Links
Bids invited for £1 million defibrillator fund
The Circuit – the national defibrillator network
Frank Pantridge – Sudden Cardiac Arrest UK
V-Fib: What Is It, Causes, Symptoms & Treatment
#TeamLAS celebrates 75 years of our NHS
Brighton Division registered on June 14th, 1915 | St John ambulance
Photos of Brighton Ambulance Service, 1946-1974 | Brighton General Hospital



